Michigan State University (MSU) researchers have created for the first time a miniature human heart model in the laboratory, complete with all primary heart cell types and a functioning structure of chambers and vascular tissue.
In the United States, heart disease is the number one cause of death. The study’s senior author and assistant professor of biomedical engineering at MSU’s Institute for Quantitative Health Science and Engineering, Aitor Aguirre, says “mini-hearts constitute incredibly powerful models in which to study all kinds of cardiac disorders with a degree of precision unseen before.”
This study, “Generation of Heart Organoids Modeling Early Human Cardiac Development Under Defined Conditions”, appears on the bioRxivpreprint server.
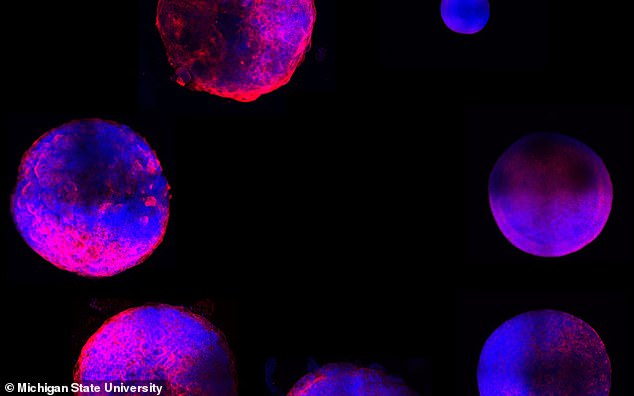
The human heart organoids, or hHOs for short, were created by way of a novel stem cell framework that mimics the embryonic and fetal developmental environments.
“Organoids, meaning ‘resembling an organ’ are self-assembling 3-D cell constructs that recapitulate organ properties and structure to a significant extent”, said Yonatan Israeli, a graduate student in the Aguirre Lab and first author of the study.
The innovation deploys a bioengineering process that uses induced pluripotent stem cells—adult cells from a patient to trigger embryonic-like heart development in a dish—generating a functional mini heart after a few weeks. The stem cells are obtained from consenting adults and therefore free of ethical concerns.
“This process allows the stem cells to develop, basically as they would in an embryo, into the various cell types and structures present in the heart”, Aguirre said. “We give the cells the instructions and they know what they have to do when all the appropriate conditions are met.”
Because the organoids followed the natural cardiac embryonic development process, the researchers studied, in real-time, the natural growth of an actual fetal human heart.
This technology allows for the creation of numerous hHOs simultaneously with relative ease, contrasting with existing tissue engineering approaches that are expensive, labour intensive and not readily scalable.
One of the primary issues facing the study of fetal heart development and congenital heart defects is access to a developing heart. Researchers have been confined to the use of mammalian models, donated fetal remains and in vitro cell research to approximate function and development.
“Now we can have the best of both worlds, a precise human model to study these diseases—a tiny human heart—without using fetal material or violating ethical principles. This constitutes a great step forward”, Aguirre said.
What’s next? For Aguirre, the process is twofold. First, the heart organoid represents an unprecedented look into the nuts and bolts of how a fetal heart develops.
“In the lab, we are currently using heart organoids to model congenital heart disease—the most common birth defect in humans affecting nearly 1% of the newborn population,” Aguirre said. “With our heart organoids, we can study the origin of congenital heart disease and find ways to stop it.”
And second, while the hHO is complex, it is far from perfect. For the team, improving the final organoid is another key avenue of future research. “The organoids are small models of the fetal heart with representative functional and structural features”, Israeli said. “They are, however, not as perfect as a human heart yet. That is something we are working toward.”
Aguirre and team are excited about the wide-ranging applicability of these miniature hearts. They enable an unprecedented ability to study many other cardiovascular-related diseases—from chemotherapy-induced cardiotoxicity to the effect of diabetes, during pregnancy, on the developing fetal heart.